
FUTURE OF HEALTHCARE SERVICES FOR THE WEST END
In everything we do, our focus is on you and the future of healthcare for our community.
6 Core Objectives
What is Healthier West End?
In 1947, “Pioneers in Rural Health” meant something different than what it does in 2022. The future of healthcare services for the West End requires us to focus on that which our founders could have never foreseen, a complex web of payment systems, rules, regulations, and the always changing landscape of rural health delivery. However, their principles grounded in community guide our expanded mission and helped to define a clear set of objectives for FCH to remain viable today and hopefully decades to come.
These include:

Objective 1
Protect and responsibly invest in the District’s health infrastructure

Objective 2
Maintain and grow financially viable services in response to community health needs

Objective 3
Deliver high-quality, safe, and person-centered wellness and healthcare in all areas of our operations

Objective 4
Create and sustain good and competitive wage jobs that fuel our local economy and provide upward economic opportunities for community members

Objective 5
Prioritize communication and collaboration with community partners to achieve improved health and wellness for ALL those who live in and love the West End!

Objective 6
Uphold a commitment to being fiscally responsible stewards of the District’s assets
Q&A
You’ve Got Questions. FCH Has Answers.
The story of Forks Community Hospital (FCH) began over 90 years ago. With the formation of the state’s first Public Hospital District in the late 1940s, FCH paved the way for rural health on the Olympic Peninsula. Whether you’re a life-long resident or new to the area, you know that FCH is a hospital and health system providing compassionate, quality-driven healthcare services to communities on the West End. What you may not know, but need to know, is that FCH is experiencing ongoing and substantial financial losses directly related to its long-term care services.
Protecting Access to Care
Protecting Healthcare for All
For decades, FCH has been operating a long-term care unit. Unfortunately, for many of these years, LTC services have lost millions of dollars because of how these services are reimbursed in the United States. While health policies negatively impact access to care for seniors across the country, it is particularly challenging for a small rural health organization like ours.
FISCALLY RESPONSIBLY LEADERSHIP
Reality of Our Current Fiscal State
After losing nearly $5 million in 2O2O and 2O2l combined from long-term care operations, the losses for 2022 will exceed $2 million. Forks Community Hospital has no choice but to take necessary action to significantly reduce the losses and strategically plan for the future of healthcare for all living and working on the West End. These losses are out of our control because Medicaid reimbursement does not even cover 50% of the cost of care.
THOUGHTFUL STRATEGIC PLANNING
Our 2021-2024 Priority Strategic Plan Goal
Assure sustainability by continually improving the financial position of the District and by achieving the financial performance ratios that will assure funds to maintain or replace facilities.
LTC operation losses will continue because the reimbursement for patient care will remain inadequate, and as such, will increase the District’s vulnerability and risks to survive.
Did You Know?
Transitioning the long-term care beds to non-skilled swing beds will allow FCH to use all beds allowed by Critical Access Hospital (CAH) participation rules. Also, by categorizing our existing long-term care beds as part of the hospital, instead of as a separate entity, they will be considered part of the hospital under the Medicare Cost Report and change the reimbursement we receive. Ultimately, this transition will stem the losses because the cost of operations will be partly covered through the Medicare Cost Report, adding about $1.8 million to narrow the $2.3 million loss.
Rural health experts from across the spectrum agree that…“few models exist that serve patient, hospital, and communities as well as the swing bed program does.”
To begin, on April 28, 2022, the FCH Board of Commissioners adopted a resolution that gives the green light to organization leaders to evaluate a plan to transition the 20 long-term nursing care beds to designated hospital non-skilled swing beds.
Don’t let the term confuse you. A “swing bed” has nothing to do with the type of bed or room a patient occupies. Instead, it relates to how patient care is reimbursed from Medicare and Medicaid by patients occupying the beds and the services provided. The swing bed program permits hospitals to use their beds interchangeably between intermediate or skilled nursing care for patients. The program started in the 1970s to address a shortage of extended care beds and under occupied hospital beds. As a result, hospitals located in rural, frontier, and underserved areas have been able to meet the need for nursing services.
Simply put, the word “swing” means that the reimbursement “swings” from billing for acute care services to billing for post-acute skilled or non-skilled nursing services, even though the patient usually stays in the same bed in the same physical location. If the patient requires more acute care, the bed can “swing” back from non-skilled to acute.
In contrast, to swing bed reimbursement, FCH’s LTC beds are limited in their use, licensed only to be utilized as they are today. In simplest terms, these beds cannot be used for any other type of inpatient care.
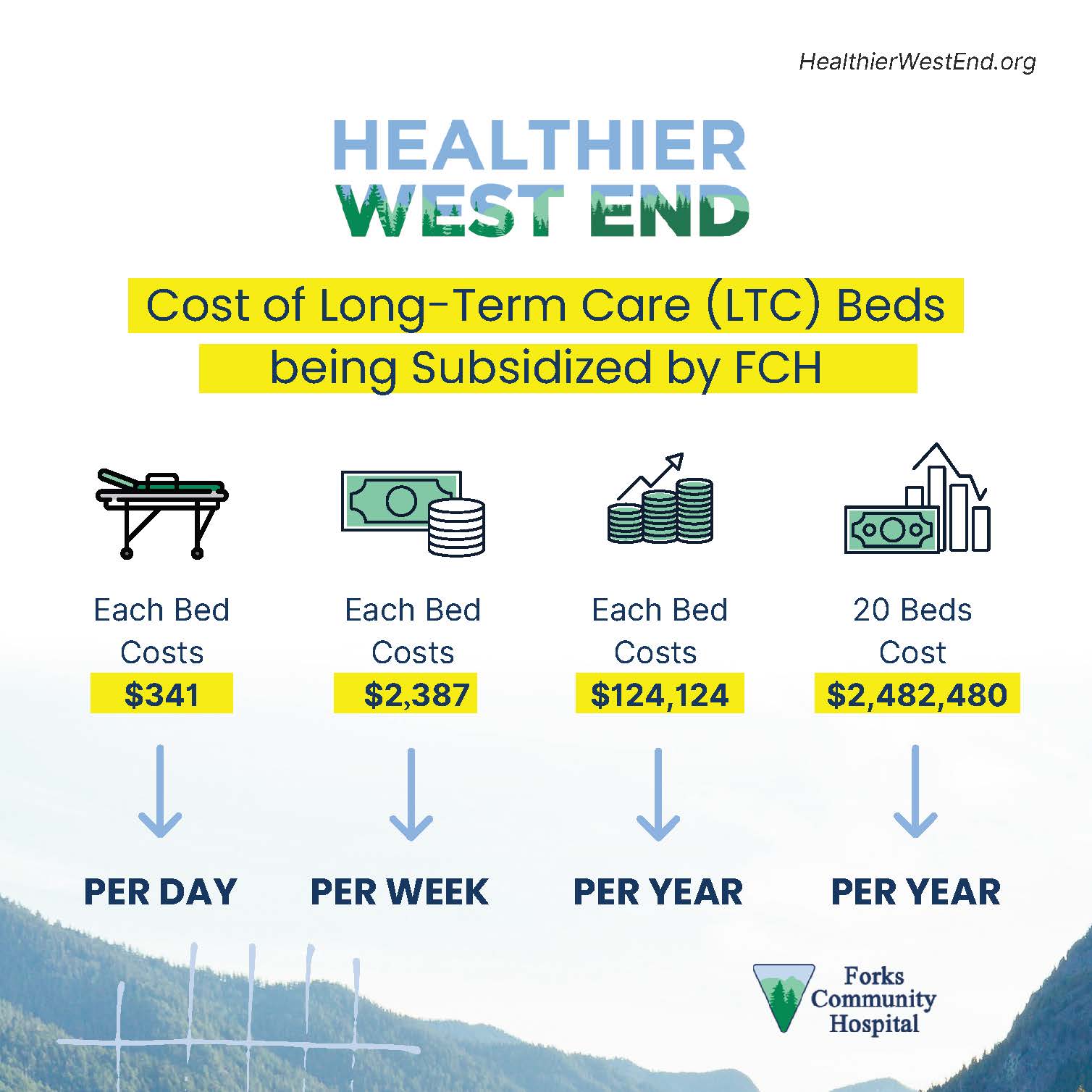
Due to the limited types of reimbursement (primarily Medicaid) these beds are eligible to receive, the 20-bed LTC unit costs FCH approximately $341 in losses per occupied bed per day. Inadequate reimbursement to cover the actual cost of care means that FCH must subsidize the operational costs of LTC at the expense of other programs and needed facility and equipment reinvestment.
Transitioning LTC beds to non-skilled swing will allow FCH to use all beds allowed by Critical Access Hospital (CAH) participation rules interchangeably for acute or post-acute care, which will change our reimbursement. In addition, by categorizing our existing LTC beds as part of the Hospital, instead of as a separate entity, they will be considered part of the Hospital under the Medicare Cost Report. This will stem the losses because the cost of operations will be partly covered through the Medicare Cost Report, adding about $1.8 million to narrow the $2.3 million loss.
FCH is one of over 1,300 CAHs in the U.S. CAH is a designation given to eligible rural hospitals by the Centers for Medicare & Medicaid Services (CMS). Congress created the CAH designation through the Balanced Budget Act of 1997 (Public Law 105-33) in response to over four hundred rural hospital closures during the 1980s and early 1990s. Since its creation, Congress has amended the CAH designation and related program requirements several times through additional legislation.
The CAH designation was designed to reduce the financial vulnerability of rural hospitals and improve access to healthcare by keeping essential services in rural communities. To accomplish this goal, CAHs receive certain benefits, such as cost-based reimbursement for Medicare services. In addition, eligible hospitals must meet the following conditions to obtain CAH designation:
- Have 25 or fewer acute care inpatient beds
- Be located more than thirty-five miles from another hospital (some exceptions apply)
- Maintain an annual average length of stay of 96 hours or less for acute care patients (this does not include swing bed patients)
- Provide 24/7 emergency care services
Yes, and in fact, FCH is one of the last remaining Critical Access Hospitals in Washington to convert its LTC beds to swing beds.
Currently, the LTC unit has 20 beds, while the hospital’s inpatient unit has 17 acute and swing beds combined (emergency room, observation, and OB beds are not included in this count.) Should the transition advance, FCH will convert an additional eight beds to swing, all beds will operate under the FCH hospital license, and the total number of available beds (acute care and swing combined) will shift from 17 to 25.
FCH does not anticipate changes to staffing (noting that currently, and due to nationwide staffing shortage, the LTC is not fully staffed), and patients can expect to receive the same high level of care and services currently provided. FCH’s average daily census (ADC), or how many beds are occupied by a patient, has historically been at four to five. This means that only four or five of our 17 Hospital beds are occupied on average. Thus, by increasing our CAH bed count to 25, we should be able to account for our ADC in Acute plus our LTC residents once they are converted to non-skilled swing.
Because CMS does not directly pay for long-term care, and reimbursements from Medicaid (which makes up for 70% of our current payer mix (2021), which is far below the actual costs to operate the long-term, FCH has experienced significant financial losses, including $2.280 million in 2020, and $2.318 in 2021. Unless a change is made, FCH expects these losses to worsen as labor and other costs increase, and reimbursement from payers remains stagnant or declines.
The nearly $5 million shortfalls of reimbursement for the essential services provided to LTC residents have required FCH to subsidize losses with revenues generated from other operations, a practice that is not sustainable nor fiscally responsible as a Public Hospital District going forward. Indeed, LTC losses, which have consistently lost money, have been detrimentally impacting the Hospital for many years and led to a lack of capital investment in the District’s facilities.
It has been suggested that FCH can simply add various outpatient and inpatient services to help subsidize current LTC operations. Unfortunately, the short answer is no; it is not possible to add services to help subsidize LTC.
Adding services that generate revenue requires market demand, growth driven by data and weighed against feasibility, significant investments, additional staffing, physical space to operate, and time to bring them online. Revenue generated from existing or new services must be reinvested into the FCH workforce, its services, and facilities and not allocated to support and supplement one service for a limited number of community beneficiaries.
The simple and definitive answer is YES! The COVID-19 pandemic has impacted FCH finances. Below is a brief breakdown of how:
First, it is widely known that in the early days of the pandemic and through 2020, hospitals and clinics across the U.S. had to cease most operations that generated the revenue that pays for staff, supplies, and essentially keeps the lights on, and doors open. As a result, rural and remote hospitals like ours especially were highly concerned about the losses, and rightfully so.
In response to the crisis, the Federal government recognized the need for organizations like ours to sustain health care services while many of their operations were interrupted for a prolonged and uncertain period.
Significant financial relief to rural hospitals came in the form of approximately $32 billion in federal support, primarily from the Provider Relief Fund (PRF), to compensate for the loss of revenue and increased expenses from the pandemic, as well as funding through the Paycheck Protection Program (PPP.) Although this support during the pandemic temporarily helped many struggling facilities, financial challenges remain across rural health care systems. For FCH, the funding was not intended to supplement for the losses in our LTC services; instead, to ensure critical aspects of the care we provide, both inpatient and outpatient, could continue.
Another significant way the pandemic has impacted FCH financials relates to our workforce. Again, it’s obvious but worth stating. Without our nurses, techs, business office staff, clinical staff, and everyone who ensures the care you need is there when you need it, FCH would be nothing but empty.
In May of 2022, the Bipartisan Policy Center published a comprehensive report focused on “The Impact of COVID-19 on the Rural Health Care Landscape.” The report sheds important light on rural workforce challenges, which were substantial before 2020, and have gotten considerably worse since the pandemic. In their report, they offer, “Rural health care systems consistently report that retaining workers and ensuring adequate staffing levels is one of their most vexing challenges. Key problems during the pandemic include staff burnout, the need of providers to leave the workforce to care for family members, and wage pressures that made it difficult for financially strapped rural hospitals to compete with other employers.” This last part is particularly relevant for FCH.
Although resources and additional funding are available to address staff burnout, fatigue, recruitment, and training, these efforts do not change the fact that FCH struggles to be competitive in compensation and wages compared to other hospitals, including other small rural hospitals, in the state. For as much as we’d like to be able to be a higher-range wage provider, our LTC losses directly impact our ability to do so. In other words, there is a direct connection between our recruitment and retention efforts and the millions of dollars in LTC losses.
No amount of relief dollars will bridge the gap of the increased wages we must pay staff to be competitive and fair. For FCH to be competitive with wages and benefits is to:
- Stem the massive and accumulating financial losses due to our LTC operations.
- Grow our provider base and recruit new providers to meet the demands of our population and increase the utilization of existing services.
- Grow our services to capture (recapture) market share, leaving our community to receive their care elsewhere.
The gap between revenue from Medicaid and self-pay and the cost of operations is simply too large. LTC’s primary expense is payroll, and labor costs have been escalating steeply for several years. Minimizing the loss would require severe staffing cuts that would be detrimental to resident care and quality. In previous years we kept labor costs lower by paying lower wages. In today’s fiercely competitive health care workforce market, and considering the remoteness of our location, and faced with a nationwide shortage of nursing staff, for example, FCH must be prepared to offer higher wages and benefits to avoid being understaffed.
The community did indeed rally behind the expansion of LTC beds back in 1984 by passing a $600,000 General Obligation Bond to construct and purchase equipment for the addition of the LTC wing of the hospital facility. They did so because, since the founding of FCH, the West End community has shown it cares deeply about taking care of each other at every stage of life. But unfortunately, the General Obligation Bond does not fund maintenance, operations, staffing, and all required to manage care for our long-term patients.
It cannot be overstated that FCH is a lifeline to care. It’s a place that offers comfort, welcomes new babies to the world, and provides a wide range of essential health services to all those who call the West End home. The FCH Board of Commissioners, leadership team, and staff want to do everything possible to ensure that FCH can continue its tradition of caring in an ever-changing and complex rural health environment. However, the investment made in 1984 was never anticipated or intended to sustain the LTC operations.
There is no debate, FCH is not in control of how its LTC patient care beds are reimbursed by Medicaid. Like every other CAH in the United States, (FCH is one of the last in Washington to make this transition) we must address the financial losses that prohibit us from being innovative in how we meet the greater care needs of all in the District.
THE FUTURE IS TODAY
Investing in Health
The Healthier West End framework is designed not just to address the challenges we face today. Our focus is to do everything possible to remain a viable public hospital despite the conditions that we have no way to control.
The healthcare industry is one of the most complicated of all. Be assured that we’re clear on our focus. Not every decision will be the most popular. Education can help bring clarity. Our most important message to our community is that a Healthier West End happens when we all work together.
- Protect and responsibly invest in the District’s health infrastructure
- Maintain and grow financially viable services in response to community health needs
- Deliver high-quality, safe, and person-centered wellness and healthcare in all areas of our operations
- Create and sustain good and competitive wage jobs that fuel our local economy and provide upward economic opportunities for community members
- Prioritize communication and collaboration with community partners to achieve improved health and wellness for the people of Forks
- Uphold a commitment to being fiscally responsible stewards of the District’s assets


FCH exists to serve nearly 10,000 people who rely on us for health services beyond inpatient care. The decision to transition the LTC beds to swing beds is the only fiscally responsible step that allows us to focus on protecting our increasingly financially vulnerable community asset and invest in our local health infrastructure.
